Navigating the complexities of mental health billing is not any small feat. Mental health providers often face an uphill struggle with regard to getting claims approved and paid by using insurance corporations. Denials can experience roadblocks to receiving compensation for offerings rendered. However, they don’t ought to be the end of the road. Effectively dealing with mental fitness billing denials and appeals requires strategy, endurance, and information on both billing techniques and insurance policies.
- Understanding Mental Health Billing Denials
- Strategies for Reducing Mental Health Billing Denials
- Navigating the Appeals Process for Mental Health Billing
- Best Practices for Managing Denials and Appeals
- The Role of Outsourcing in Denial and Appeal Management
- The Importance of Persistence in Appeals
- Conclusion
Understanding Mental Health Billing Denials
Common Reasons for Denials
Denials show up for several motives, but some are more unusual than others. Identifying the foundation reason for denials permits you to keep away from them in destiny.
- Coding Errors
One of the most frequent causes of mental health claim denials is coding errors. Incorrect use of ICD-10 or CPT codes or failing to match the correct diagnosis to the service provided can lead to immediate rejections.
- Insufficient Documentation
Another main motive is incomplete or insufficient documentation. Insurers require particular notes and assisting documents to justify the clinical necessity of the remedy supplied.
- Coverage Issues
Sometimes, the difficulty stems from the patient’s coverage plan not overlaying particular mental health offerings. It’s vital to affirm coverage earlier than rendering services to avoid this type of denial.
How Denials Affect Mental Health Practices
Denials can considerably effect the monetary fitness of a exercise. If left unmanaged, they lead to lost revenue, wasted time, and delivered strain for group of workers. Knowing how to cope with denials successfully can help practices get better payment and keep economic stability.
Strategies for Reducing Mental Health Billing Denials
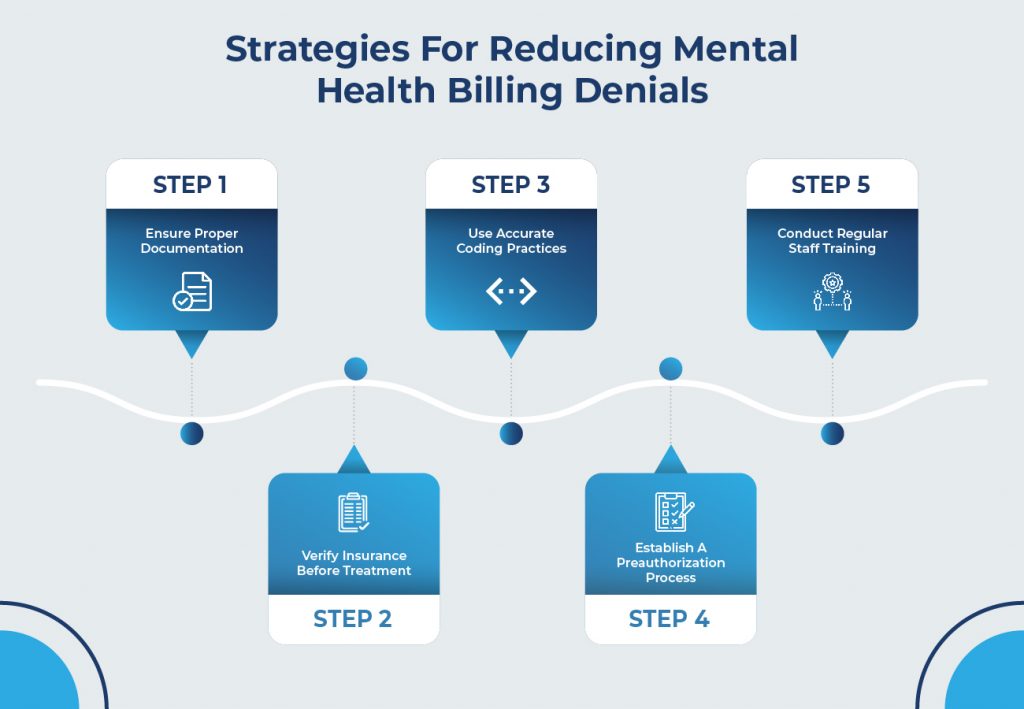
Ensure Proper Documentation
Proper documentation is the backbone of a successful billing process. Ensure that all clinical notes, treatment plans, and patient records are thorough and up to date.
- Importance of Thorough Patient Records
Accurate and detailed patient records support claims and help justify the services provided. They also serve as evidence in case of an appeal.
Verify Insurance Before Treatment
Verifying a affected person’s insurance coverage earlier than beginning treatment can prevent many denials related to insurance or eligibility.
- Confirming Patient Eligibility
Confirming a patient’s insurance info and coverage guarantees that the services you offer are covered by means of their plan, minimizing the hazard of insurance-based denials.
Use Accurate Coding Practices
Coding mistakes can lead to costly denials, so it’s important to use the correct ICD-10 and CPT codes.
- ICD-10 and CPT Codes
Make sure your team is familiar with the latest coding guidelines and uses the most accurate codes for each service provided.
Establish a Preauthorization Process
Preauthorization can save time and reduce denials by ensuring the insurance company approves a service before it is rendered.
- Why Preauthorization Matters
Getting preauthorization helps to secure payment for high-cost or recurring treatments and prevents later disputes with the insurance company.
Conduct Regular Staff Training
Training staff regularly on coding changes and compliance updates helps prevent errors and denials from occurring.
- Training on Compliance and Coding Updates
Stay on top of industry changes by scheduling training sessions to keep your staff updated on the latest billing rules and coding standards.
How Outsourced Medical Billing Services Can Benefit Your Practice
Navigating the Appeals Process for Mental Health Billing
Steps to Take After Receiving a Denial
The first step in dealing with a denial is to understand why it happened. Carefully review the denial notice to determine what went wrong.
- Review the Denial Reasons
Each denial will come with a reason code explaining the cause. Understanding these reasons is crucial to submitting a successful appeal.
Submitting a Strong Appeal
An appeal is your chance to correct any errors or provide additional information that supports your claim. Writing a clear, concise, and compelling appeal letter is essential.
- Writing an Effective Appeal Letter
Make sure your appeal letter includes all the necessary documentation and clearly addresses the reason for the denial.
Follow-Up After Submission
Don’t just submit the appeal and forget about it. Follow up with the insurance company regularly to track the status of your appeal.
- Tracking Your Appeal Status
Use billing software to track your appeal and ensure that nothing slips through the cracks. Follow up with the insurer if you don’t receive a timely response.
Best Practices for Managing Denials and Appeals
Maintain Clear Communication with Insurance Providers
Establishing open lines of communication with insurance providers helps avoid misunderstandings and can speed up the resolution of denials.
Use Billing Software to Track Claims
Modern billing software can help track claims and denials, making it easier to spot patterns and identify common reasons for rejections.
Develop a Denial Management Workflow
Having a structured denial management process ensures that denials are addressed quickly and systematically, preventing them from piling up.
The Role of Outsourcing in Denial and Appeal Management
Why Outsource Denial Management?
For a few practices, outsourcing denial control can be a valuable and powerful way to deal with billing complexities while freeing up time for clinical work.
Choosing the Right Outsourcing Partner
When outsourcing, it’s essential to select an accomplice who is aware of mental health billing and has an established song file in lowering denials.
The Importance of Persistence in Appeals
Don’t Give Up After the First Denial
Persistence is prime while handling denials. Don’t surrender if your first appeal is rejected—many successful appeals take more than one round of returned-and-forth with the coverage agency.
Document Every Step of the Process
Keeping precise facts of each verbal exchange and submission for the duration of the appeals process is crucial for protecting your exercise and increasing the possibility of a hit final result.
Conclusion
Managing mental health billing denials and appeals may be difficult; however, with the proper strategies in the region, it’s possible to lessen the range of denials and improve your achievement price in appeals. By ensuring accurate documentation, verifying insurance coverage, and staying persistent, intellectual fitness practices can preserve monetary health and attention to handing over high-quality care.
