Nephrology medical billing and coding can be a complex field, given the unique nature of kidney-related treatments. This specialization requires attention to detail, accuracy, and a deep understanding of nephrology-specific codes and procedures. Without proper billing and coding strategies, nephrology practices can face claim denials, revenue loss, and compliance risks. In this article, we will cover key strategies to ensure effective nephrology medical billing and coding, helping practices improve their financial health and streamline operations.
Understanding Nephrology Billing and Coding
What is Nephrology Medical Billing?
Nephrology billing entails filing correct claims for kidney-associated remedies, consultations, and strategies to insurance organizations. It’s critical for shooting revenue, as nephrology treatments such as dialysis, kidney transplants, and control of persistent kidney disease (CKD) require specialized billing know-how.
What is Nephrology Coding?
Nephrology coding refers to the assignment of specific codes, such as CPT and ICD-10, to represent medical diagnoses and procedures related to kidney diseases. Coders must ensure the correct use of these codes to avoid errors, delays, or denials in reimbursement.
Why Specialized Billing and Coding Matter in Nephrology?
Due to the chronic nature of kidney diseases and the frequency of treatments like dialysis, nephrology billing and coding require precision. Specialized knowledge helps ensure accurate reimbursement and compliance with insurance and regulatory requirements, minimizing the risk of denials and financial setbacks.
Key Strategies for Effective Nephrology Billing
Streamlining Documentation Processes
- Ensuring Accurate and Complete Documentation
Accurate documentation is the foundation of successful nephrology billing. Providers must ensure that all treatments, consultations, and procedures are properly documented. Any missing or incomplete information can lead to claim denials.
- Importance of Electronic Health Records (EHR)
Reducing errors in documentation is greatly facilitated through the use of EHR systems. EHRs offer standardized templates and streamlined patient data entry, ensuring that accurate and easily accessible data for billing purposes is provided.
Using Nephrology-Specific Codes Correctly
- Nephrology Procedure CPT Codes
For nephrology therapy, accurate CPT coding is crucial. Dialysis management codes (such as 90935 90937) and consultation codes for kidney disease diagnosis and treatment are important nephrology CPT codes.
- Nephrology Conditions’ ICD-10 Codes
Chronic kidney disease (N18.1–N18.9) is one of the nephrology-related diseases represented by ICD-10 codes. Maintaining correct ICD-10 coding is essential for recording patient diagnoses and obtaining the right compensation.
Right Charge Capture
Ensuring accurate charge capture is essential for properly recording all billable services provided by nephrologists. Any missing or incorrectly entered rates can lead to lost revenue. By implementing a strong charge capture system, we can ensure that every service provided is billed accurately.
Provider and Billing Team Communication
It is essential to maintain open and effective communication between nephrology companies and billing groups to ensure accurate documentation and coding of all services. Holding regular meetings to address common billing issues can greatly enhance accuracy and efficiency.
Strategies for Nephrology Coding
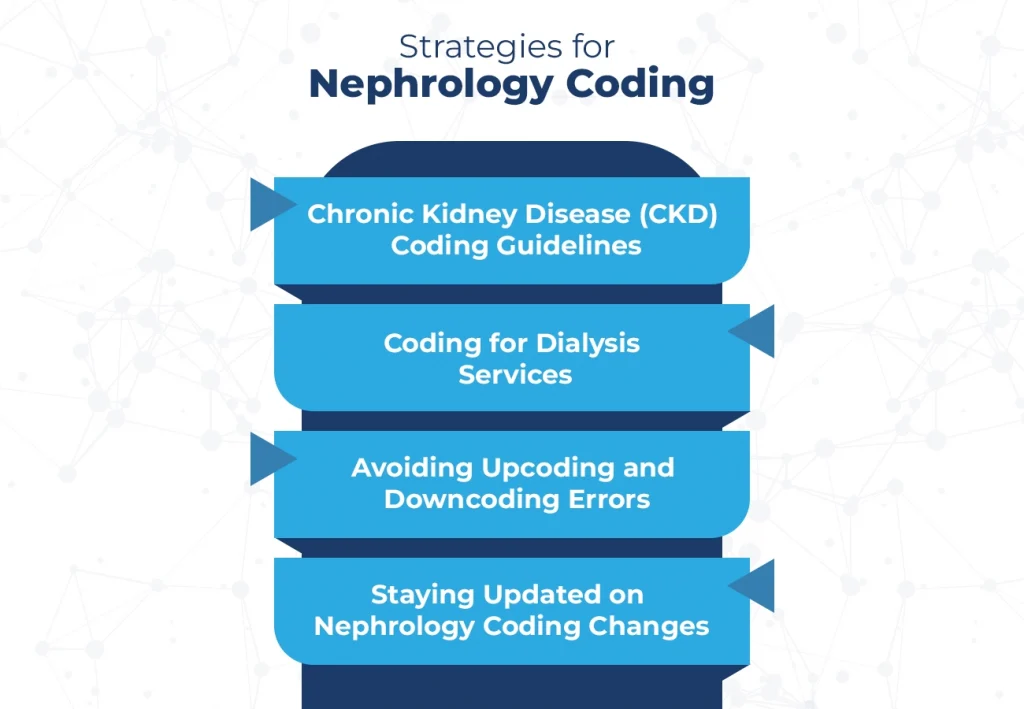
Chronic Kidney Disease (CKD) Coding Guidelines
Coding for CKD requires an understanding of the specific stages (from N18.1 for stage 1 CKD to N18.9 for stage 5 CKD). Using the appropriate ICD-10 code is vital for accurate diagnosis documentation.
Coding for Dialysis Services
Dialysis coding can be complicated, with different codes based on the type and frequency of dialysis treatments. Codes like 90935 (single evaluation) and 90937 (multiple evaluations) must be used correctly to ensure proper reimbursement.
Avoiding Upcoding and Downcoding Errors
Remember that both upcoding and downcoding can result in compliance issues. It’s crucial for coders to be well-versed in compliance rules and to steer clear of these errors to guarantee the accurate processing of claims.
Staying Updated on Nephrology Coding Changes
As coding guidelines frequently change, it’s essential for nephrology billing staff to undergo continuous training. Staying updated on new codes and regulations ensures accurate billing and reduces the risk of denials.
Best Practices for Denial Management in Nephrology Billing
Scaling claim denials in nephrology results from improper documentation, coding inaccuracies, and insurance requirements not being met. In order to prevent denials, you first need to know what the root causes are.
Prior Auths and Eligibility Checks
It has a huge impact on cutting down claim denials by verifying the patient’s eligibility and preauthorization of nephrology treatments before delivery. This step will ensure that the treatments are covered by the insurance plan of patients.
How to Write A Successful Appeal Letter
If your claim is denied, you will need to submit an appeal with the appropriate appeal letter. Ensure that the appeal is supported by relevant documents and clearly explains why you are requesting a reassessment of the claim.
Conclusion:
Specialized expertise, meticulous attention to detail, and the utilization of contemporary technologies are necessary for efficient nephrology medical billing and coding. Nephrology practices may improve their revenue cycle and lower the likelihood of claim denials by putting best practices in documentation, coding, denial management, and compliance into practice. The adoption of billing software and ongoing employee training may improve the accuracy and efficiency of billing even more.
