A large number of healthcare practices rely on a medical billing clearinghouse to handle their insurance claims efficiently. But what exactly is a medical billing clearinghouse? And why is it considered a wise investment for healthcare providers? Read on to discover comprehensive answers to these and more inquiries.
Topics
What is a Medical Billing Clearinghouse?
Medical billing procedures can be complex and demanding. However, utilizing an intermediary clearinghouse service provider can greatly simplify this process. This type of service can efficiently review claims for inaccuracies, maintain comprehensive records for each claim, and facilitate electronic funds transfer (EFT) payments. Ultimately, this results in a higher rate of timely claim payments and reduces the amount of time wasted due to avoidable misunderstandings.
How Does a Medical Billing Clearinghouse Work?
At the point when medical services suppliers set up medical billing software, each guarantee is changed into a record called an ANSI-X12-837. Each document is then shipped off the clearinghouse and completely audited to guarantee there are no blunders. When blunder-free, the record is safely communicated to the insurance agency for handling, all in consistency with the guidelines of the Health Insurance Portability and Accountability Act (HIPAA).
Benefits of Using a Medical Billing Clearinghouse?
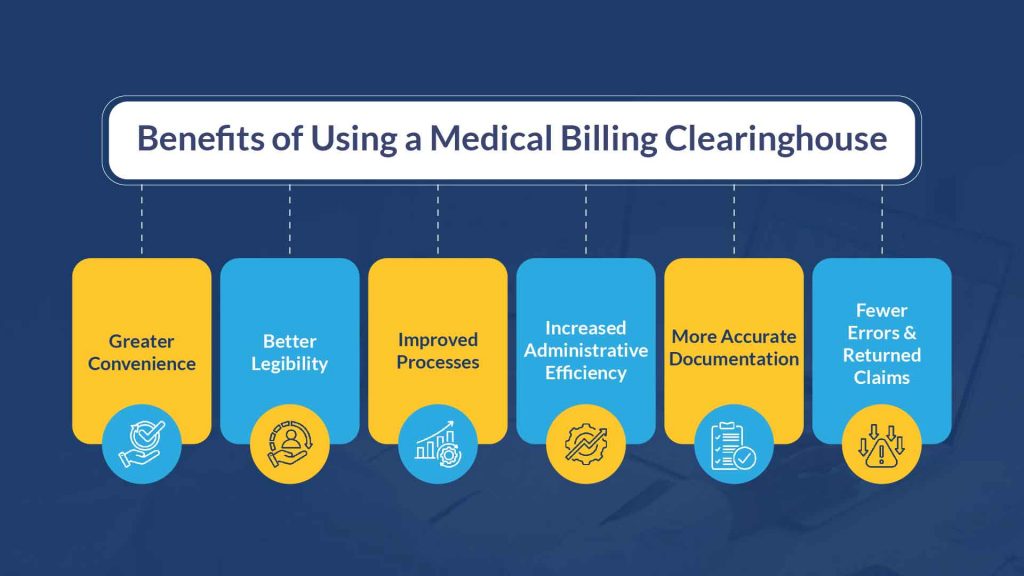
There are many benefits to utilizing a medical billing clearinghouse for your claims process. Here are only a couple of key advantages that come from utilizing this choice:
- Greater Convenience
Most of the medical services claims are currently handled electronically rather than through the mail. Federal medical insurance and other huge protection payers like to utilize electronic clearinghouses to filter through and review claims. Electronic entries make the whole claims process faster and smoother.
Also, medical billing programming accomplices commonly supply patient gateways that assist clients with overseeing solutions, lab results, and correspondence. Patients can undoubtedly get to these entries from their PC, tablet, or cell phone.
- Better Legibility
Specialists and other clinical experts are not known for the lucidity of their handwriting. With an arrangement of electronic clinical records set up (as regulated by a clearinghouse supplier), insurance agency can undoubtedly peruse patient information. This guarantees that cases will not be dismissed in view of an incorrectly spelled patient name or other preventable mistakes.
- Improved Processes
Numerous medical services suppliers need to move a case’s data to their charging programming, print the claim out as a CMS1500 structure, and afterward mail it to the fitting insurance agency. After the safety net provider gets the case, they review it for mistakes. Assuming they view it as any, they send the claim back to the supplier, and the billing staff is starting over.
Every one of these requires some investment and labor. Interestingly, the utilization of a clinical billing clearinghouse can save you and your staff from contributing information and, once again, losing valuable time fixing botches. Fundamentally, you’re in a superior situation to zero in on quiet consideration as opposed to essential, however dreary, desk work.
- Increased Administrative Efficiency
Medical care suppliers and insurance payers each utilization billing programming, however the two projects may not be viable with one another. This can bring about the two sides investing an unnecessary measure of energy physically entering in information. In any case, when the two sides utilize a clearinghouse that can overcome any barrier between each piece of programming through electronic information reconciliation (EDI), the correspondence cycle between payer and supplier turns out to be much faster and easier.
Also, when you acknowledge electronic remittance advice (ERA) from your clearinghouse and EFT installments from your protection payers, your claims cycle will accelerate, you will not need to stress over lost desk work or taken checks, and your staff will actually want to zero in on assignments that are more significant for your tasks and main concern. Indeed, even the time saved from sending/getting paper mail or physically finishing bank store exchanges can increase efficiency for your staff.
- More Accurate Documentation
The American Medical Association has assessed that roughly 42% of doctors will eventually confront a clinical negligence guarantee in their profession. While there’s very little you can do to accelerate the lawful cycle around a misbehavior suit once started, a medical billing clearinghouse supplier can facilitate a portion of your weight by giving point-by-point and precise data on the case being referred to. What’s more, you’ll have the option to rapidly get to that data as conditions direct.
- Fewer Errors and Returned Claims
By far, most billing issues and returned claims come from human mistakes. The U.S, as a matter of fact. The government Responsibility Office observed that more cases are denied due to charging mistakes and qualification inquiries than on the grounds that the insurance agency differs in the need for the consideration that the patient got. Additionally, medical billing mistakes and different issues make medical care suppliers lose an expected $125 billion every year.
Clearinghouses audit bills and claims for errors such as:
- Missing patient information
- Inaccurate patient information (incorrectly spelled name, wrong birthdate, and so forth.)
- Incorrect insurance provider data
- Mistaken billing codes (inaccurate Spot of Administration, HCPCS, or CPT codes, and so on.)
- Fragmented information connected with systems or diagnostics performed
- “Double-billing” for a similar help
Improved ROI
Healthcare providers who utilize a trusted medical billing clearinghouse witness a substantial enhancement in their return on investment. Here are just a few compelling reasons why:
- Clearinghouse programming can recognize mistakes like a flash and caution your staff right away, which permits them to rapidly make changes while the data is still new in their brain.
- A clearinghouse stores individual payer data so information connected with that payer doesn’t need to be reemerged each and every time, making the accommodation interaction a lot quicker.
- You have the choice to send every one of your cases without a moment’s delay as opposed to presenting a different record for every single payer.
- On account of a crisis occasion, a clearinghouse can furnish you with a back-up duplicate of any significant charging information you submitted and afterward lost.
- You get a good deal on printing ink, stamps, mailing supplies, and different costs related with paper correspondence.
How to Choose the Right Medical Billing Clearinghouse Provider?
Selecting the right medical billing clearinghouse provider is crucial for your practice’s success. Each clearinghouse offers distinct services and benefits. Here are five key factors to evaluate when choosing a clearinghouse:
1. Evaluate Your Options
Make sure to thoroughly research multiple options. When exploring various possibilities, ensure you are fully informed and equipped to answer critical questions, such as:
- What is the degree of this clearinghouse’s compass (neighborhood, local, public)?
- Are my training’s protection payers on their rundown?
- Does this clearinghouse offer internet-based admittance for following and refreshing submitted claims?
- Do they charge for their administrations consistently, or do they charge per accommodation?
- Does their help group examine dismissed claims?
- If a protection payer requires paper-based claims, will the clearinghouse handle that correspondence too?
Considering these questions will assist you in refining your search criteria and arriving at a well-informed decision.
2. Focus on Customer Support
The best clearinghouses are those that deal with quick and responsive client care. Outsourcing the technical and managerial parts of your case interaction to an outsider is useless in the event that your staff needs to look out for the telephone for quite a long time just to get a solution to a key case-related question.
Considering that, search for a clearinghouse that offers every minute of everyday support and has the capacity to answer any request in no less than a day or less. Ensure the clearinghouse has a devoted specialized helpline. Go over the clearinghouse’s standard agreement with absolute attention to detail to figure out what level of client assistance they will ensure.
3. Investigate Claim Response Times
One of the essential benefits of utilizing a medical billing clearinghouse is quick case reaction time. As a rule, one ought to know every day whether a claim has been acknowledged or returned because of blunders. To lessen pointless postponements, search for a clearinghouse that offers speedy updates on individual cases.
4. Verify Fast Turnaround Time for 835s
HIPAA orders that medical care insurance suppliers convey an 835 transaction set while paying suppliers, alongside a clarification of advantages (EOB). Some clearinghouses will not send 835s to suppliers for a very long time after an exchange has been finished. Others might charge extra for ERA 835s.
Interestingly, the best clearinghouses will immediately send you the 835s and EOBs that match your finished exchanges at no additional cost to you. Confirm that the clearinghouse has the capacity to do this, as well as a demonstrated history of doing as such.
5. Consider Usability
At long last, contemplate how easy to use the clearinghouse’s product will be for your staff. Much of the time, different staff individuals will expect admittance to claims data. An excessively confounded or irrational program will steepen your staff’s expectation to learn and adapt and probable reason a larger number of blunders than a less complex piece of programming would.
Likewise, you ought to check the program’s similarity with your ongoing cases charging programming. You likewise need to ensure that your clearinghouse permits you to affirm patient qualification continuously, and gives a strong and broad web index for information access. You may likewise need to explore progressed highlights, for example, dismissal examination, optional cases handling, and free action synopses.
Bottom Line
Basically, a medical billing clearinghouse can make your claims accommodation process smoother, more precise, more proficient, and less tedious. Assuming you pick the right clearinghouse for your training, you’ll almost certainly see prompt advantages from using this choice.
Where to Get the Advanced Claim Scrubbing Solutions
When you select RCM Matters as your medical claims clearinghouse, you’re choosing a cutting-edge, compliant, and efficient solution to streamline and enhance your medical billing processes.
Here’s why choosing us is the best strategic decision for your healthcare organization:
Our team comprises professionals with in-depth knowledge of CPT, ICD-10, and HCPCS Level II coding systems and deep familiarity with payer-specific rules, ensuring accurate and compliant medical claim submission.
Experience seamless integration with top Electronic Health Record (EHR) systems through HL7 interface standards. This means smoother data exchange, quick claim submission, and instant claim status tracking for a hassle-free experience.
Our system meets the stringent data security and privacy requirements of HIPAA. All PHI is handled securely to ensure your organization’s compliance with regulatory standards.
We offer a cost-effective solution with a transparent fee structure, removing the need for separate charges for eligibility verification, a service usually outsourced by other clearinghouses.
Count on our expert customer support team to streamline your EDI transactions and resolve any 837P and 837I claim form issues you encounter.
Our advanced software carefully reviews claims to catch errors such as missing modifiers, incorrect diagnosis codes, and inaccurate patient identifiers before submission. This significantly lowers the chances of denials or rejections, ultimately enhancing your clean claim rate.
We provide automated, real-time checks for patient eligibility, reducing the risk of claim denials due to coverage issues and contributing to more efficient revenue cycle management.
Need help or additional information? Our sales representatives are here for you! Contact us
