On the surface, laboratory billing can seem straightforward, but the truth is rather different. It entails a complicated series of procedures and rules that, if not followed properly, may result in lost money and problems with compliance. Like any healthcare service, laboratories depend on precise billing to keep things running smoothly and to be financially stable. Correct billing is essential whether you operate a clinical diagnostics center, a pathology lab, or specialist genetic testing services.
Importance of Efficient Laboratory Billing
Getting paid on time is only one aspect of efficient laboratory billing; other goals include maintaining accuracy, cutting down on delays, and skillfully handling denials. A lab’s revenue cycle may be greatly increased, and regulatory compliance can be guaranteed with a simplified billing procedure. On the other hand, ineffective billing may result in denied claims, postponed payments, and even legal issues.
Understanding the Laboratory Revenue Cycle
The laboratory revenue cycle encompasses everything from patient registration to the collection of payments. Understanding how this cycle works is key to improving billing efficiency.
- Overview of Key Components
Patient intake, which includes confirming insurance coverage and gathering the required personal data, is where the revenue cycle starts. Test orders, coding processes, claims submission, and payment reconciliation follow.
- Common Challenges in Lab Billing
Labs face unique challenges, such as managing complex insurance networks, handling a high volume of claims, and adhering to ever-changing regulatory standards. Addressing these challenges head-on is crucial for minimizing billing errors and maximizing revenue.
Step-by-Step Laboratory Billing Process
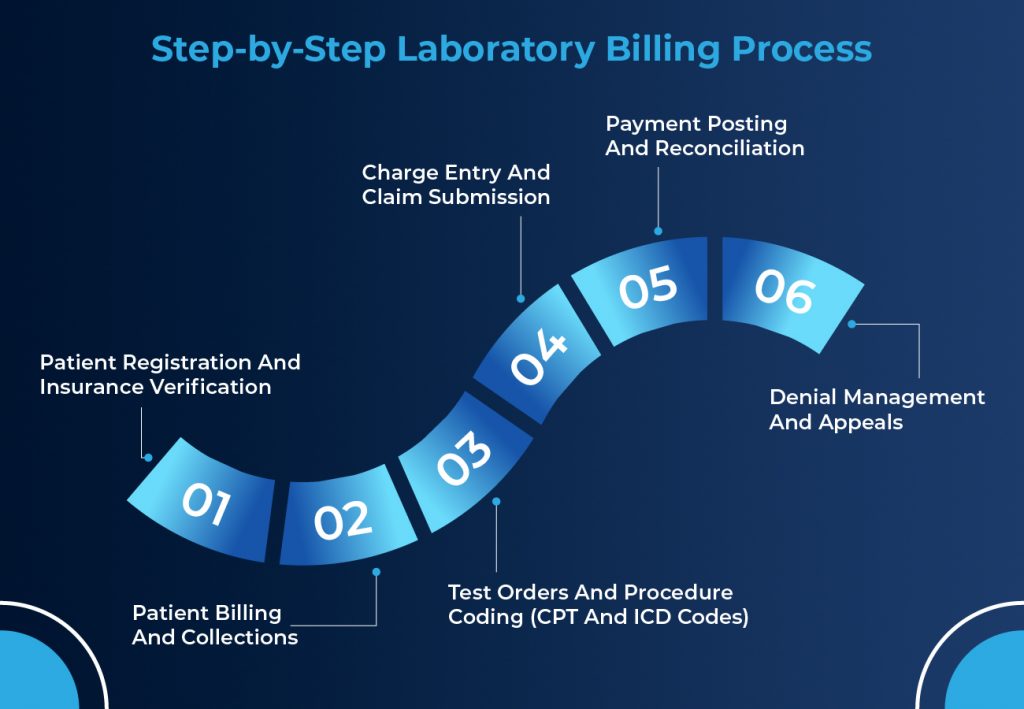
- Patient Registration and Insurance Verification
The first step in the billing process is patient registration, where the lab gathers essential details such as patient demographics and insurance information. Insurance verification is critical here—without it, your lab could be performing services that won’t be reimbursed.
- Test Orders and Procedure Coding (CPT and ICD Codes)
After a test is ordered, the laboratory must assign the appropriate Current Procedural Terminology (CPT) and International Classification of Diseases (ICD) codes. These codes must be accurate and up-to-date as they determine how insurance companies reimburse the lab.
- Charge Entry and Claim Submission
Once coding is complete, the next step is charge entry, where the lab’s services are recorded for billing. Claims are then submitted electronically to insurance companies, ensuring they include all required documentation.
- Payment Posting and Reconciliation
To ensure that everything was paid appropriately, payments must be posted accurately and reconciled with the original claim. To prevent income loss, any disparities should be fixed as a result.
- Denial Management and Appeals
Denial management involves reviewing any rejected claims and determining the reason for denial. If necessary, appeals should be submitted to challenge these denials, improving the chances of reimbursement.
- Patient Billing and Collections
Finally, if a balance remains after insurance, patient billing kicks in. Clear communication with patients about their outstanding balances and payment options is essential for successful collections.
How Outsourced Medical Billing Services Can Benefit Your Practice
Why Accuracy in Coding Matters
- Avoiding Rejections and Denials
One of the main reasons for denied claims is coding problems. Ensuring that CPT and ICD codes are entered accurately can prevent denials and speed up the reimbursement process.
- Enhancing Revenue Through Proper Coding
Accurate coding not only reduces the risk of denials but also ensures your lab is being reimbursed for all the services provided. Under-coding can lead to revenue loss, while over-coding can trigger audits and penalties.
Key Regulatory and Compliance Considerations
The Health Insurance Portability and Accountability Act (HIPAA) mandates strict patient privacy standards. Compliance with these regulations during the billing process is essential to avoid hefty fines and legal issues.
Laboratories must also adhere to specific billing guidelines set by Medicare and Medicaid. Understanding these guidelines is key to successfully submitting claims for reimbursement.
The Role of Medical Billing Software in Laboratory Billing
Automated billing software simplifies many of the tasks involved in laboratory billing, from coding and claim submission to payment posting and denial management. Automation can drastically reduce errors and improve efficiency.
When choosing billing software, look for features like customizable coding templates, real-time eligibility verification, and robust reporting tools that can help track revenue and improve your lab’s financial performance.
How Outsourcing Laboratory Billing Can Improve Efficiency
Advantages of Outsourcing
Outsourcing laboratory billing to a third-party carrier can relieve your group of the executive burden, allowing them to be aware of patient care. Additionally, billing specialists can lessen claim denials and speed up the sales cycle.
How to Choose the Right Billing Partner
Look for a billing partner with experience in laboratory services and a proven track record of reducing denials and increasing collections. Ensure they’re informed about cutting-edge regulations and industry trends.
Improving Revenue Cycle Management (RCM) in Labs
Metrics for Monitoring RCM Success
Keep an eye on metrics like claim denial rates, days in accounts receivable (AR), and the percentage of collections as a way to measure the health of your lab’s revenue cycle.
Streamlining Lab Operations for Better Billing
Streamlining inner approaches, enhancing the team of workers’ schooling, and adopting superior billing technology are all ways to enhance the overall revenue cycle management of your lab.
Common Laboratory Billing Errors and How to Avoid Them
Incorrect patient information, coding issues, and missed receipt deadlines are just a few examples of common billing mistakes. Employee training and regular audits can help reduce these errors.
Tips for Enhancing Laboratory Billing Efficiency
Investing in the ongoing education of your billing staff can drastically improve your lab’s billing accuracy and efficiency. Keep them up-to-date on regulatory changes and coding updates.
Keeping Up with Regulatory Changes
Healthcare regulations are constantly evolving, and staying compliant is crucial. Regularly review new rules and ensure your billing processes align with current standards.
Pathology, Genetics, and Other Specialty Laboratory Billing
Every laboratory specialization has different billing difficulties. For instance, pathology laboratories take care of extra complex check requests, whereas genetics labs would possibly have to cope with extra charges and longer declared processing periods.
The Future of Laboratory Billing: Trends and Innovations
Telemedicine and Remote Lab Billing
As telemedicine becomes more common, remote laboratory services are on the rise. Labs will need to adapt their billing processes to handle remote testing and the regulatory nuances that come with it.
The Impact of AI and Machine Learning
Artificial intelligence (AI) and system-gaining knowledge are starting to play a widespread role in automating and enhancing the accuracy of laboratory billing. These technologies will probably continue to adapt and reshape the billing landscape.
Conclusion
Streamlining your laboratory billing process is key to optimizing revenue and reducing operational headaches. By ensuring accuracy in coding, adopting automated billing solutions, and staying up-to-date with industry regulations, labs can improve their revenue cycle management and avoid common pitfalls.
