Think of medical billing like putting together a puzzle. Each piece represents a step in the billing process, working together to make sure everyone gets what they need. From the moment you visit the doctor to the time the bill is paid, every step matters.
In this guide, we’ll take you through the basics of medical billing in 2024. Whether you’re new to the field or just want to understand how it all works, this guide is here to help you navigate the world of medical billing simply and clearly. Let’s get started!
Medical billing is about organizing and sending claims to insurance companies or government health programs. It can be tricky because it involves turning medical services, treatments, and diagnoses into standardized codes using systems like Current Procedural Terminology (CPT) and International Classification of Diseases (ICD) codes. These codes act like a common language, making sure everything is accurate, following the rules, and transparent when it comes to money matters. They also help healthcare providers get paid for the services they provide.
The first stage of the medical billing process is patient registration, which aims to gather and confirm important patient entry and history data. This includes establishing an electronic health record (EHR), verifying insurance coverage, and obtaining personal information. This stage creates a thorough patient profile, which paves the way for correct invoicing.
Front desk operations involve vital tasks like appointment scheduling, collecting co-pays, and updating records. Smooth interactions and accurate invoicing stem from effective front desk operations, which also handle initial consultations. During these sessions, thorough assessments are conducted, decreasing claim denials by ensuring precise coding aligns with procedures rendered.


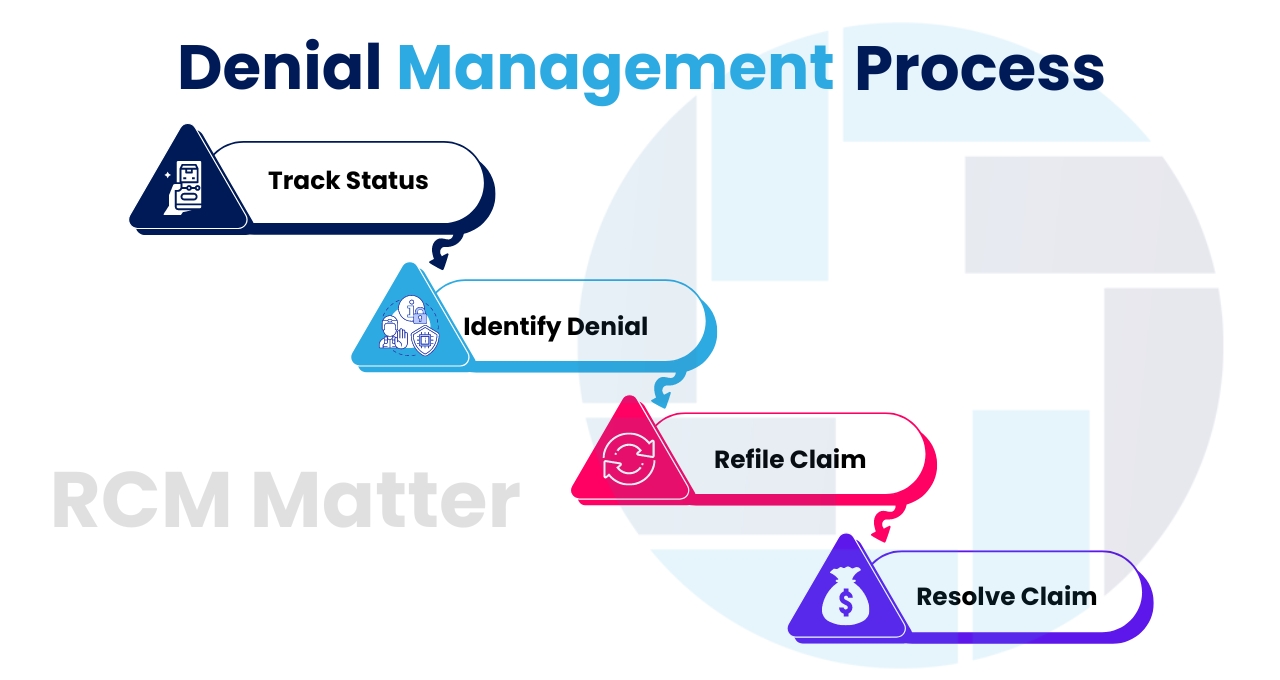
Identification and examination of denied claims are steps in the Denial Management Services, after which rectified claims are resubmitted. This phase involves the following steps:
Optimize billing, claims and collections with expert RCM support let our professionals handle the process so you can focus on patient care.


