CPT (Current Procedural Terminology) codes are essential for accurately reporting medical services and procedures to insurance payers. Within the context of nursing facility care, CPT codes 99304 through 99318 cover a wide range of services. From initial and subsequent evaluations to discharge planning and annual assessments, these codes cover all.
This blog is tailored for medical billers, coders, healthcare providers and administrators working in or with nursing facilities. It breaks down the nuances of each CPT code within the 99304–99318 range, providing practical tips for documentation, compliance and claim accuracy. This guide will also cover how services for medical billing and coding in California can assist providers in effective financial management. Medical Coding Services may not only increase revenue, by reducing coding error and claim denials but also streamline billing process. k
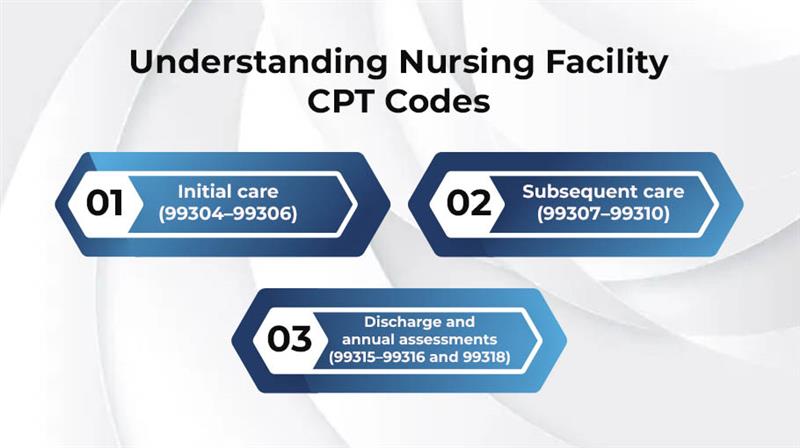
CPT codes 99304–99318 are used to report evaluation and management (E/M) services provided to patients in nursing facilities. These codes are divided into three main categories:
Initial care (99304–99306)
Subsequent care (99307–99310)
Discharge and annual assessments (99315–99316 and 99318)
Accurate documentation is crucial when billing these codes. The provider must clearly demonstrate the level of history taken, examination performed and complexity of medical decision-making (MDM).
Initial nursing facility care codes are used for the patient’s first comprehensive assessment upon admission.
99304: Low complexity – requires detailed history and exam and straightforward or low-complexity MDM.
99305: Moderate complexity – includes comprehensive medical history and exam of the patient and moderate MDM.
99306: High complexity – involves a comprehensive history, comprehensive exam and high-complexity MDM.
The admitting provider must perform the initial assessment.
All three components (history, exam and MDM) must meet or exceed the stated requirements.
Document the reason for admission, current medical status and plan of care.
These codes cover follow-up visits during the patient’s stay.
99307: Problem-focused history and exam, straightforward MDM.
99308: Expanded problem-focused, low-complexity MDM.
99309: Detailed history and exam, moderate-complexity MDM.
99310: Thorough medical history and exam, complex MDM.
Based on the patient’s diagnosis or condition, these CPT codes are generally used on a daily or weekly basis.
The frequency of visits should be justified by the condition and diagnosis of the patient.
Link each visit to the current care plan.
Ensure the documentation reflects changes in the patient’s condition or treatment.
Discharge services codes are used on the day a patient leaves the facility.
99315: Discharge lasting 30 minutes or less.
99316: Discharge lasting more than 30 minutes.
A final examination of the patients and a summary of their stay.
Include medication reconciliation, a formal procedure of comparing patient pre-admission and recent lists of medicines.
Instructions for follow-up care can help ensure continuity of care and provide the patient with clear expectations for ongoing management.
Information about coordination with other providers, for instance, primary care specialists or physicians, if applicable.
CPT 99318 is used to report an annual nursing facility assessment. This assessment includes a comprehensive medical review of the patient’s medical status, including history and a very thorough examination, typically performed by the attending the physician.
Comprehensive medical history and proper examination.
Update or renewal of care plans.
Unlike subsequent care visits, this is a planned, comprehensive annual medical service, not based on changes in the conditions.
Selecting a code that doesn’t match the documented level of service. Avoid this by following CMS E/M guidelines.
Ensure all components of the code level are met and recorded.
Nursing facility care typically uses a Place of Service (POS) code of 31. Ensure modifiers are used properly when multiple providers are involved.
One of the primary hurdles for medical billing is the complexity of managing multiple insurance providers. Healthcare providers face many challenges in medical billing, including denied claims, coding errors and slow reimbursement, particularly in California. California expert medical billers allow healthcare providers to spend more time with patients without stressing about cash registration. Here are the following ways for effective coding and reimbursement.
Medical coding rules do change frequently. For accurate coding and compliance, always review the latest updates from organizations like CMS.
Always use the correct code sets for diagnoses (ICD-10-CM) and treatment (CPT).
Tailored prompts and templates help ensure that you capture all required documentation.
Routine chart reviews can catch coding or documentation issues early, reducing the risk of denials or audits.
Accurate coding using CPT codes 99304–99318 is essential for effective nursing facility billing. It ensures compliance, streamlines reimbursement and delivers nop notch care by understanding the distinctions between initial, subsequent, discharge and annual services. Avoiding common billing errors, expert medical billers, providers and coders can streamline documentation and billing processes.
Q: What documentation is needed for 99306?
A comprehensive history and physical exam, plus high-complexity MDM. Documentation should clearly show the complexity and justification for the service level.
Q: How often can 99318 be billed?
Once annually per patient, typically aligned with the patient’s admission anniversary or care review cycle.
Q: Can these CPT codes be used for assisted living facilities?
No. CPT 99304–99318 are intended for nursing facilities (SNFs and NFs), not assisted living.
Optimize billing, claims and collections with expert RCM support let our professionals handle the process so you can focus on patient care.
