Imagine completing a patient visit, only to find that your claim was denied because of a single incorrect code. For many healthcare practices, this situation is all too common. Accurate coding is the foundation of effective medical billing and determines whether claims are processed correctly and records remain reliable.
Outsourced medical coding services can help your practice ensure accurate coding. They can handle CPT and ICD-10 codes accurately while providing practical insights that support your day-to-day work. These services enable you to manage claims efficiently, monitor service patterns, and maintain reliable records without placing additional strain on your staff.
This post explains an important aspect of medical coding: CPT and ICD-10 codes, highlighting their differences and how they work together, as well as the advantages of engaging professional medical coding services for your practice.
Medical coding employs a standardized language to document diseases, procedures, and services offered by practices. In simple terms, it answers two key questions: why the patient received care and what service was provided.
CPT codes record procedures, tests, and services performed during a patient encounter. Examples include evaluation-and-management (office) visits, lab tests, imaging studies, injections, and surgical procedures. CPT data helps practices track service mix, measure utilization, and inform staffing and scheduling decisions.
CPT is a system of five-digit numeric codes maintained by the American Medical Association (AMA). These codes cover a broad spectrum of healthcare services, including:
Some commonly used CPT codes include:
CPT codes clarify the services provided during a patient encounter and allow insurers to interpret care accurately. They are also valuable for understanding practice activity. Proper coding helps practices:
Incorrect or missing codes can slow claim processing, create administrative bottlenecks, and complicate record-keeping. Outsourced medical coding services can help practices use correct CPT codes, providing reliable data for operational decisions.
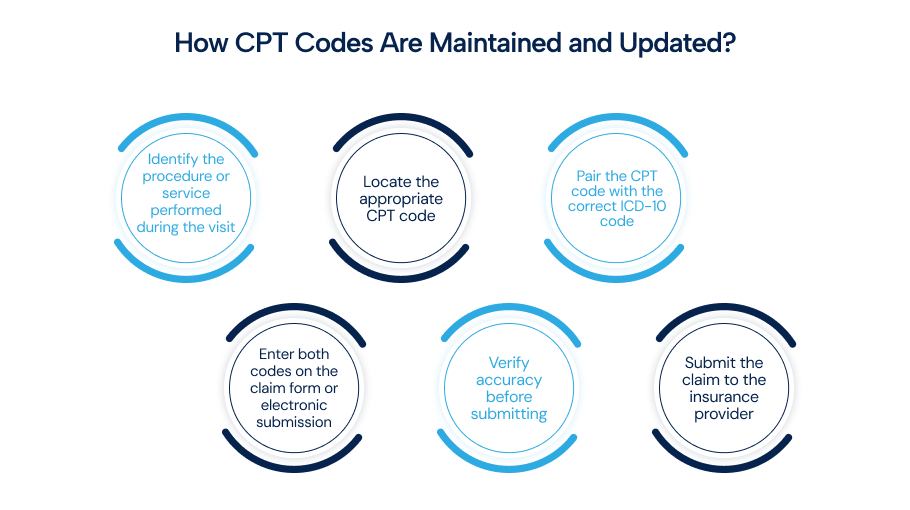
The AMA updates CPT codes on January 1 each year. New codes are introduced, and some are revised or removed. Each update may introduce new codes, modify existing ones, or remove outdated codes. Keeping your codes up to date is essential to avoid billing errors. Updated codes can be accessed through EHR systems, AMA manuals, or the official AMA website.
ICD-10 codes document the patient’s condition or reason for care. Diagnosis codes justify tests and treatments for example, a hypertension code supports management, and they enable trend analysis, chronic-disease monitoring, and reporting.
The WHO publishes the international ICD classification, while the U.S. clinical modification, ICD-10-CM, is maintained by the National Center for Health Statistics (NCHS/CDC) and implemented in coordination with CMS. ICD-10-CM uses alphanumeric codes to standardize diagnoses across settings.
ICD-10 codes cover chronic conditions, injuries, infections, and mental health disorders. Common examples include:
Codes may include additional characters (up to 7 in ICD-10-CM) to capture laterality, severity, episode, or complications, improving specificity for payment, reporting, and clinical analytics.
U.S. updates to ICD-10-CM are published annually and take effect on October 1. Use current code sets, since outdated codes can lead to rejections, delayed payments, and additional administrative work. Updated code sets are available via EHR vendors, the CDC/NCHS website, CMS resources, and official codebooks.
Simple steps to use ICD-10 codes:
The table below summarizes the main differences between CPT and ICD-10 codes:
|
Feature |
ICD-10-CM |
CPT |
|
Purpose |
Diagnosis/reason for care |
Procedure/service performed |
|
Shows |
Why was treatment needed |
What service was done |
|
Format |
Alphanumeric (up to 7 characters in ICD-10-CM) |
Numeric (most are five digits) |
|
Maintained by |
NCHS/CDC (U.S. clinical modification) / WHO (international) |
American Medical Association (AMA) |
|
Example |
E11.9 – Type 2 diabetes without complications |
99213 – Established patient office visit |
|
Annual update |
October 1 (ICD-10-CM) |
January 1 (CPT) |
ICD-10-CM codes document the diagnosis or reason for the encounter. CPT codes describe the procedures, tests, or services performed. Submitting both codes on a claim shows payers what was done and why, which supports medical necessity and reduces avoidable denials.
Example:
A patient with Type 2 diabetes seen for a routine visit might be coded as:
Keeping code sets current and ensuring complete documentation are the top operational issues practices often face. Complex encounters with multiple diagnoses or bundled services require careful sequencing and, in some cases, modifier use. Regular audits and focused clinician–coder reviews reduce errors.
Many practices engage in medical coding outsourcing to access experienced coders, reduce internal staffing burdens, and improve claim accuracy. When evaluating outsourced medical coding services, review accuracy metrics, audit support, EHR integration, turnaround times, and payer appeals capabilities.
Accurate coding is critical for all healthcare practices. U.S.-based practices seeking solutions for medical billing and coding in California can benefit from outsourcing their coding tasks to medical coding agencies to maintain up-to-date codes, reduce errors, and ensure reliable billing.
Effective medical coding solutions also enable practices to manage operations more effectively while maintaining precise claims. Whether you need full outsourcing or targeted support, RCM Matter delivers medical coding services to physician practices, outpatient clinics, and community hospitals. Our team of certified coders provides precise, compliant coding to help maximize your revenue.
Get in touch with RCM Matter today to discuss your needs and secure top medical coding services.
What is Clinical Documentation Improvement (CDI) and why does it matter?
CDI programs improve the detail and clarity of clinician notes so coders select the most specific codes, reducing denials and strengthening medical-necessity support.
How are telehealth visits coded differently from in-person care?
Telehealth uses the same CPT/ICD structure but often requires place-of-service modifiers, documentation of the virtual medium, and consent.
What is SNOMED CT, and how does it relate to ICD/CPT?
SNOMED CT is a clinical terminology used in EHRs for detailed documentation. Mappings (crosswalks) translate SNOMED concepts into ICD or CPT codes for billing and reporting.
What role do automated claim edits play?
Edit systems (NCCI, MUEs, payer edits) block incompatible code pairs or excess units, preventing improper payments but requiring coding and appropriate modifiers to justify services.
How are experimental or investigational services handled in coding?
Such services must be documented clearly and often use specific HCPCS or temporary CPT codes. Prior authorization and clear documentation are critical to avoid denials.
Optimize billing, claims and collections with expert RCM support let our professionals handle the process so you can focus on patient care.
