Accounts Receivable (AR) represents the outstanding payments healthcare providers are entitled to for the services they deliver. However, collecting these payments is not always straightforward. Delays, denials and administrative errors can significantly affect a practice’s revenue. Utilizing Accounts Receivable Follow-Up Services ensures that unpaid claims are tracked efficiently, denials are addressed promptly and reimbursements from both payers and patients are received on time. For new and established healthcare practices alike, effective AR follow-up is essential to maintaining financial stability, reducing revenue leakage and improving cash flow.
AR follow-up involves monitoring unpaid claims, communicating with insurance companies and ensuring accurate payment posting. It is a vital part of revenue cycle management (RCM) and directly impacts a practice’s bottom line.
AR specialists handle following tasks such as.
Tracking and resolving unpaid or delayed claims with insurance companies before they reach timely filing limits.
Identifying reasons for claim denials such as coding errors or missing documentation and resubmitting corrected claims.
Communicating with patients about outstanding balances in a clear and professional manner to prevent confusion or disputes.
Accurately recording payments and ensuring they match payer remittances to prevent discrepancies.
Proactive follow-up reduces delays in insurance reimbursements helping practices get paid sooner.
By addressing errors quickly, practices can correct and resubmit claims before deadlines.
Consistent follow-up ensures predictable revenue which is critical for day-to-day operations.
Regular AR management prevents accounts from aging beyond recovery, reducing financial losses.
Transparent and timely billing minimizes patient frustration and improves the overall experience.
Accurate follow-up ensures that claims are submitted correctly and comply with payer rules, reducing the risk of audits or penalties.
The following are the practices that lack structured AR processes face.
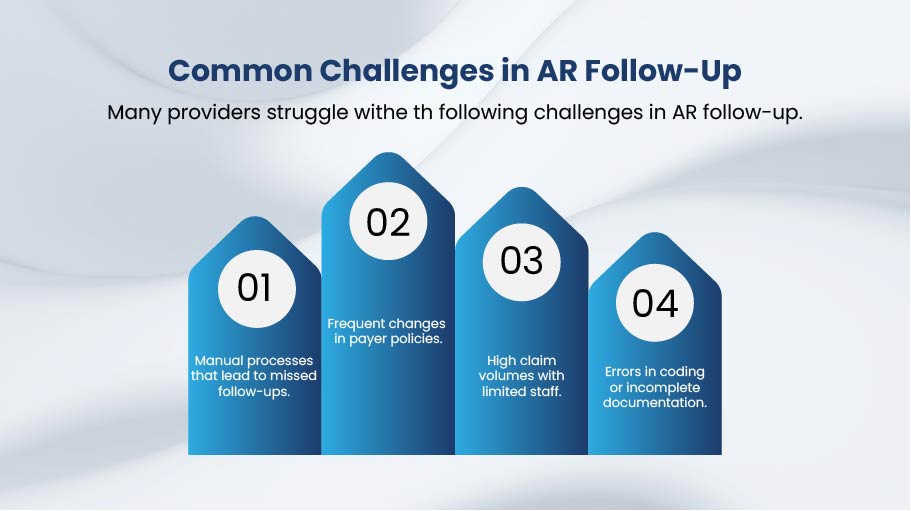
Many providers struggle withe th following challenges in AR follow-up.
To improve collections and reduce denials, practices should follow these best practices.
Using medical billing software with AR tracking features can streamline workflows, reduce errors and ensure timely follow-up. Integration with EHR systems allows practices to track claims, payments and patient balances in one place improving efficiency and accuracy.
For many practices, especially new or growing ones, handling AR in-house can be time-consuming and costly. Outsourcing accounts receivable to a professional billing partner offers several advantages:
By partnering with companies that provide accounts receivable follow-up services, healthcare providers can focus on delivering quality care while ensuring their revenue cycle remains healthy and compliant.
What is AR follow-up in medical billing?
AR follow-up is the process of tracking unpaid claims, addressing denials and ensuring healthcare providers receive timely reimbursement from insurance companies and patients.
Why is AR follow-up important for healthcare providers?
It ensures faster payments, reduces claim denials, improves cash flow and minimizes revenue loss due to unpaid or delayed claims.
How do Accounts Receivable Follow-Up Services help?
These services provide expert support for tracking and collecting unpaid claims, managing denials and improving overall revenue recovery for healthcare practices.
When should a practice consider outsourcing accounts receivable?
Practices should consider outsourcing if they face high claim volumes, frequent denials or lack in-house staff to manage AR efficiently.
What are the benefits of outsourcing AR follow-up?
Outsourcing offers faster collections, reduced administrative burden, lower overhead costs and access to experienced AR specialists who understand payer rules.
AR follow-up is not just an administrative task. It is a critical component of a practice’s financial success. Effective AR management ensures faster payments reduces denials and strengthens patient satisfaction.
For practices struggling with collections or facing high claim volumes, outsourcing account receivable can be a cost-effective solution. By leveraging expert accounts receivable follow-up services, healthcare providers can achieve higher reimbursement rates, improved cash flow and a more efficient revenue cycle.
Optimize billing, claims and collections with expert RCM support let our professionals handle the process so you can focus on patient care.
